 In 1890, Von Mering and Minkowski discovered that removing the dog's pancreas can cause the dog to develop diabetes, which for the first time really links the cause of diabetes to the pancreas. However, in 1898, Zuelzer and other scholars attempted to use pancreatic extracts to treat diabetes but failed to succeed, causing serious allergies and local purulent infections. Over the next 20 years, a large amount of experimental evidence has gradually gathered, and it is found that the cause of diabetes is the pancreatic endocrine islets, which can secrete a “factor†that regulates blood glucose homeostasis. In 1920, Canadian Toronto surgeon Banting and assistant Best ligated the dog's pancreatic ducts to make pancreatic acinar atrophy, extracted cooled extract from the atrophied pancreas, and injected it into the diabetic dog. It was found that the dog's blood glucose was indeed obvious. decline. With the help of biochemist James Collip, Banting and Best improved the extraction and purification of pancreatic extracts, greatly reducing the toxic side effects of the extract. In January 1922, Banting and Best injected Leonard Thompson, a 14-year-old diabetic patient with a pancreatic extract, at the Toronto General Hospital. The patient’s blood glucose levels dropped to normal levels. They named the extract insulin and publicly reported to the conference at the American Association of Physicians in Washington, DC, on May 3, 1922. It was recognized by everyone and considered to be the greatest achievement in the history of modern medicine. Banting received the 1923 Nobel Prize in medicine.
In 1890, Von Mering and Minkowski discovered that removing the dog's pancreas can cause the dog to develop diabetes, which for the first time really links the cause of diabetes to the pancreas. However, in 1898, Zuelzer and other scholars attempted to use pancreatic extracts to treat diabetes but failed to succeed, causing serious allergies and local purulent infections. Over the next 20 years, a large amount of experimental evidence has gradually gathered, and it is found that the cause of diabetes is the pancreatic endocrine islets, which can secrete a “factor†that regulates blood glucose homeostasis. In 1920, Canadian Toronto surgeon Banting and assistant Best ligated the dog's pancreatic ducts to make pancreatic acinar atrophy, extracted cooled extract from the atrophied pancreas, and injected it into the diabetic dog. It was found that the dog's blood glucose was indeed obvious. decline. With the help of biochemist James Collip, Banting and Best improved the extraction and purification of pancreatic extracts, greatly reducing the toxic side effects of the extract. In January 1922, Banting and Best injected Leonard Thompson, a 14-year-old diabetic patient with a pancreatic extract, at the Toronto General Hospital. The patient’s blood glucose levels dropped to normal levels. They named the extract insulin and publicly reported to the conference at the American Association of Physicians in Washington, DC, on May 3, 1922. It was recognized by everyone and considered to be the greatest achievement in the history of modern medicine. Banting received the 1923 Nobel Prize in medicine. First, animal insulin and human insulin era
In the more than 60 years after the discovery of insulin, the source of insulin is mainly extracted from the pancreas of pigs and cattle. Due to insufficient purification of the original insulin preparation, it is prone to allergic reactions, repeated occurrence of drug resistance, hyperglycemia and hypoglycemia, and hypodermic lipoatrophy at the injection site. Or hyperplasia, in addition to a large variation in potency between different batches. With the advancement of protein purification technology, people can obtain more purified “unimodal insulin†or “monocomponent insulinâ€, but due to differences in the molecular structure of human insulin and swine and insulin, they still can not solve the problem of immunogenicity. problem. This period was known as the era of animal insulin.
In the late 1970s, gene recombination technology became mature and perfect. In 1978, human insulin was successfully synthesized using genetic engineering technology. Its primary, secondary, and tertiary structures are identical to those of human insulin, and have been confirmed to have complete biological functions. In 1982, Eli Lilly developed the world's first genetically engineered synthetic human insulin, Humulin R, and it was successfully launched. This epoch-making product is the first peptide biomedical product synthesized by humans and the synthesis of human insulin. The animal insulin immunogenicity problem is solved, insulin allergy and antibody production are greatly reduced, and the bottleneck of animal insulin production is also solved.
Physiological insulin secretion includes the two parts of insulin secretion during mealtime and basal insulin secretion in non-feeding state. Whether it is animal insulin or human insulin, by adding zinc ions to the formulation or combining it with protamine, the time for subcutaneous absorption of insulin can be prolonged significantly, and the action time can exceed 10-24 hours, thereby serving as basal insulin. The development of these preparations completely averted the worries of patients with type 1 and type 2 diabetes, and also led to a satisfactory control of blood sugar in most diabetic patients, delaying the occurrence of complications.
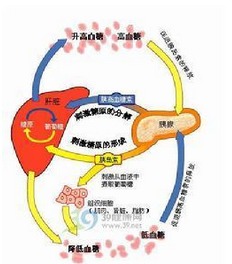
However, rapid insulin secretion after eating in the physiological state, first to reach the liver portal vein system, rapid suppression of glycogen output, which is extremely important for controlling postprandial blood glucose fluctuations, but whether the injection of animal short-acting insulin or human short-acting insulin must first be the first Then to the portal vein system, and only 30min after the short-acting insulin injection gradually began to work, the peak time of 2 ~ 4h, duration of up to 6 ~ 8h, apparently can not be a good simulation of physiological postprandial insulin secretion. Physiological basal insulin secretion is very stable, the action curve is flat, there is no obvious peak effect, and both the long-acting protamine zinc human insulin (PZI) and the intermediate effect protamine zinc insulin (NPH) have obvious absorption peaks. And pharmacokinetics and pharmacodynamic studies have found that the absorption and effect of these two kinds of insulin vary within and between individuals. Due to these limitations of short-acting insulin, PZI, and NPH, blood glucose control in patients fluctuates and the risk of hypoglycemia is high.
Second, the era of insulin analogues
The insulin molecule present in the solution is a hexamer formed by two insulin molecules forming a dimer and then three dimers and two zinc ions forming a symmetrical arrangement around the triad, so after injection subcutaneously, the insulin hexamer Gradually dissociate into monomer to absorb into the blood. Through continuous research on the primary structure, spatial three-dimensional structure and insulin function of insulin molecules, it was learned that several amino acids of insulin near the C-terminus of the A-chain and the N-terminus of the B-chain are involved in the affinity of insulin and its receptor; while the B-chain is close Several amino acids at the C-terminus, especially B28 and B29, are involved in the polymerization of amino acids and insulin molecules. Therefore, genetic engineering or other molecular biology methods can be used to modify the insulin molecule and increase or decrease the interpolymerization ability of insulin molecules so as to obtain an ultra-long-acting or ultra-short-acting insulin analogue that meets clinical needs, and biological activity and immunity. The originality remains unchanged.
The currently available short-acting insulin analogues include insulin levulinum, insulin aspart and insulin glulisine. The short-acting insulin analogues are superior to ordinary human short-acting insulin long-acting insulin in pharmacokinetic and pharmacodynamic properties. Taking aspart insulin as an example, the abdomen is injected subcutaneously with large doses of insulin aspart or soluble human insulin 0.2 U/kg. The peak concentration of insulin aspart is twice that of soluble human insulin, and aspart insulin has decreased after 60 minutes of injection. Soluble human insulin did not begin to decrease until 180 min after injection; in the first 2 h, the area under the aspart antibiotic-hour curve (AUC) was twice that of soluble human insulin, but there was no difference between the 10 h AUC. The pharmacodynamic study of the glucose clamp technique showed that the maximum glucose infusion rate (GIR) was reached - half aspart insulin was 20 min earlier than soluble human insulin, and GIR was reduced from peak to 50% as early as insulin insulin 80 min earlier than soluble human insulin . Therefore, short-acting insulin can better simulate the effects of prandial insulin.
The long-acting insulin analogues, insulin glargine and insulin detemir, have a duration of up to 24 hours, have a stable effect, have less variation in the effect between individuals than NPH, and are less likely to produce hypoglycemia, and are better basal insulin preparations. However, current long-acting insulin analogues and short-acting insulin analogues cannot be made into premixed preparations.
Third, the future long-acting insulin preparations
1.insulin degludec: degludec is the removal of threonine B30 threonine, a 16-carbon fatty acid by glutamic acid and human insulin B29 lysine connected to the formation of long-acting insulin analogues. Degludec insulin exists as a double hexamer in the formulation. After injection into the skin, due to the rapid dispersion of phenol, the unique side chain structure of degludec insulin (glutamic acid and fatty acids) makes it easy to form multi-hexamer chains in the presence of zinc ions. Later, with the slow diffusion of zinc ions, multiple hexamer chains slowly dissociate into dimers and monomers and absorb human circulation through capillary walls [5]. The formation of multi-hexamer chains is the most important mechanism of its delayed action. In addition, the chain structure of fatty acids makes it possible to reversibly bind to albumin, which further delays the action. Degludec has an elimination half-life of more than 25 hours and an effective duration of more than 40 hours. In a 16-week multicenter randomized controlled clinical trial, 245 patients with type 2 diabetes were treated with metoclopramide combined with degludec on a daily basis, three times per week, or once daily insulin glargine at the end of the trial. There was no significant difference in blood glucose profiles between the 3 groups of HbAlc and 9-day day, but the rate of hypoglycemia in the degludec daily group was significantly lower than that of the degludec three times per week or the insulin glargine once daily group. Recently, two multi-center, randomized, open-label treatment trials for 1 year in patients with type 1 diabetes and type 2 diabetes were published on Lancet, comparing dregec and insulin glargine to meal insulin reduction, respectively Sugar curative effect. Regardless of type 1 or type 2 diabetes, the decrease in HbAlc was similar at the end of the treatment in both groups, but the fasting plasma glucose was lower in the degludec group than in the insulin glargine group, and there were fewer overall and nocturnal hypoglycemic events. Unlike existing long-acting insulin analogues, degludec can be pre-mixed with short-acting insulin analogues and has fewer hypoglycemic events than pre-mixed insulin 30.
2. Humalog-PEG (LY2605541): humalog-PEG is a polyglycol molecule with a relative molecular weight of 20000 covalently bonded to lysine at position B28 of Ummira, resulting in a macromolecule of approximately 75,000, exceeding that of white. Protein, injected slowly into the skin, slowed down the elimination of the kidneys, the half-life of the effect can be as long as 2 ~ 3d, and the role of the variability is very low. Because of its larger molecular structure, its molecular structure also changes its distribution in the tissues. It is easily phagocytosed by the sinusoidal epithelium in the body, and therefore is distributed in the liver at a higher concentration than peripheral tissues. Theoretically, it can provide more physiological insulin. supplement. A 12-week, multinational, multicenter, randomized, controlled n-phase clinical trial showed that the ratio of huraalog-PEG to insulin glargine was similar for fasting blood glucose and HbA1c reduction, but the former had a 48% reduction in the risk of hypoglycemia at night. The body weight of the insulin glargine group decreased by an average of 0.84 kg. On the other hand, it was also found that liver transaminase levels in the humalog-PEG treatment group increased significantly within the reference range of normal value, and the glycerol triacetate level also increased significantly (mean increase of 0.4 mmol/L for men and 0.3 mmol/L for women). .
3. Biodel Long-acting Basal Insulin: Biodel is a bio-tech company specializing in the modification of peptides and proteins. The company's "BIOD-adjustable basal insulin" is a patented GRAS excipient in insulin glargine. It can change the action time of glargine and make it longer or shorter. Adapt to the different needs of different patients for basal insulin action time, and have a more gentle, more stable pharmacokinetic characteristics. Another pre-clinical "BIOD-smart basal insulin" newly developed by Biodel can change with different levels of glucose in the surrounding tissues. Its main formula is insulin glargine, glucose oxidase and peroxidase (pH 4). We know that the solubility and absorption rate of insulin glargine is pH-dependent, and the lower the pH, the more easily dissociated insulin glargine into monomer and absorb. When the glucose level in the interstitial fluid is increased, the above reaction system will generate more gluconic acid, and the pH of the microenvironment will decrease, which will increase the absorption of insulin; otherwise, the blood glucose will decrease, the production of gluconic acid will decrease, and the pH of the microenvironment will increase. Reduce insulin absorption. This pharmacodynamic profile has been confirmed in pig in vivo tests.
4.SraartInsulin: This is another possible "smart" basal insulin developed by SmartCells. This glucose-reactive insulin principle is: insulin can compete with glucose and a patented compound "SmartInsulin polymer" reversibility After the injection of Smart Insulin into the skin, the glucose in the interstitial fluid can displace insulin from the polymer binding site into a free state and be absorbed into the blood. The higher the blood glucose is, the more insulin is displaced.
5. FT105: FT105 is a long-acting basal insulin based on its original "Medusa Drug Delivery Platform" by Flamel High Tech. Medusa is a biodegradable polymer linked to vitamin E with a polyglutamic acid chain. After being mixed with peptides or protein drugs in aqueous solution, the two are non-covalently bonded to form a nanohydrogel. When injected into the skin, a "depot" is formed, after which the drug is gradually displaced by the protein in the tissue fluid and absorbed, and the effect is stable for up to 14 days. FT105 uses recombinant human insulin combined with Medusa's drug platform to make insulin more smooth in human body and lasting longer than 48 hours. Steady insulin levels can be achieved within 3 to 4 days after injection. Intra-individual variation is very small and hypoglycemic events can be significantly reduced. There was no adverse reaction in the injection. Because Medusa is biodegradable to glutamic acid and vitamin E in vivo, it has high safety.
Fourth, the future of ultra-short-acting insulin preparations
1. Recombinant human hyaluronidase and short-acting insulin analogues (rHuPH20-insulin): Hyaluronic acid is one of the components of the extracellular matrix, which forms a natural barrier under the skin and prevents the injected drug from spreading to Qualitative tissue, thereby slowing the absorption of drugs from the capillaries. Hyaluronidase catalyzes the hydrolysis of P-1,4 glycosidic bonds between N-acetylglucosamine and glucuronic acid residues in hyaluronic acid, degrades long-chain hyaluronic acid, lowers its viscosity, and increases tissue permeability. . Therefore, hyaluronidase can be combined with other drugs to increase drug diffusion and absorption rate. rHuPH20 is a recombinant human hyaluronidase that can be combined with current insulin products (including recombinant human insulin and fast-acting insulin analogs) to form a cocktail, allowing more rapid absorption and faster onset of action of insulin or insulin analogues. The shorter the time, the lower the variability of insulin action between individuals and individuals. A double-blind, six crossover trial in 14 healthy volunteers compared the pharmacokinetics of three fast-acting insulin analogues (insulin aspartate, insulin glulisine, lispro insulin) with or without rHuPH20. Pharmacodynamic parameters, the results show that combination of rHuPH20 can make fast-acting insulin analogs onset time 13-25min faster, the action time shortened 40 ~ 49min.
2. Linjeta and BIOD-123: Linjeta is a patented prototype of an ultrashort-acting insulin based on human insulin that was originally developed by Biodel Biopharmaceutical Co., Ltd., also known as “VIAjectâ€. It was submitted to the US FDA for a new drug application in December 2009, but Unapproved, the FDA requires the addition of two key Phase 1H clinical trials. In 2011, Biodel reinvented the prototype formulation, and developed two new formulae, BIOD-123 and BIOD-125. Phase I clinical trials showed that the peak time of BIOD-123 and BIOD-125 was nearly 1 compared with lispro insulin. More than doubled, the local response at the injection site was similar and it appeared that BIOD-123 was better tolerated. A phase II clinical trial comparing randomized, open-label BIOD-123 and insulin lispro participated in 30 centers in the United States. Case recruitment was completed at the end of March 2013 and results will be announced by the end of September 2013.
V. Other routes of administration of insulin
Because of the psychological fear and invariability that insulin injections cause to patients, scientists have been working on the possibility of non-injectable routes of administration such as oral or sublingual preparations (IN-105, 4-CNAB, VIAtab , Oraliri, etc.), transdermal drug delivery preparations, but these administration methods have the disadvantages of low bioavailability, weak hypoglycemic efficacy, and large intra-individual variability, which are currently unable to meet clinical needs. Another possible route of administration is an insulin inhalation formulation. The first insulin inhalation formulation “Exubera†was listed in 2006, but the manufacturer will withdraw from the market after 1 year for commercial or other reasons. Compared with subcutaneous injections of conventional insulin or insulin lispro, Exubera has a rapid onset, rapid peak (about 49 minutes), and short duration. Theoretically, inhaled insulin is more suitable for the supplement of prandial insulin, but the general bioavailability of inhaled insulin is low, generally only 8% to 15%. Afrezza is MannKind's unique "Technosphere" insulin powder for inhaled insulin, its bioavailability can be as high as 24% to 28%, peak time of about 14min, duration of 2 ~ 3h. A recently published 52-week m-phase clinical trial M participated by 10 countries showed that Technosphere inhaled insulin and insulin aspart 30 have similar hypoglycemic effect (average reduction of HbAlcO 68%), and mild to moderate The incidence of hypoglycemia and severe hypoglycemia was significantly lower than in the control group. It is the most likely inhaled insulin to be listed in the near future.
In conclusion, insulin therapy has made tremendous progress over the past 90 years. The original animal insulin rescued the lives of countless diabetic patients; genetic recombinant human insulin overcomes the immunogenicity; human insulin analogues better simulate the physiological insulin secretion pattern, which is more convenient and safer; the next generation is more effective in fast meal times Insulin and long-acting basal insulin are expected to provide more stable blood glucose control, fewer hypoglycemic reactions, and reduce the complications and mortality of diabetes; and inhaled or oral insulin may provide more friendly to some patients Drugs to improve the quality of life of patients.
Durable Aluminum Rollator with Seat: Stylish and modern aluminum rollator rolling walker features a durable frame, padded seat and backrest, and a spacious storage pouch
4 wheels rollator :8-inch wheels and soft-grip tires are perfect for indoor/outdoor use
Sturdy and Lightweight: the portable rollator is easy to transport; built for everyday use with a weight capacity of 300 poundsAdjustable Fit: Rollator`s easy-turn lever allows you to quickly adjust the height of the ergonomic handles; height-adjustable rollator also includes a removable hinged backrest that can be folded up or down for easy storage
Rollator walker folding: Rollator walker with side-to-side folding design allows easy folding with one hand and maintains a standing position, making this folding walker exceptionally easy to roll, park, and store anywhere
Aluminum walker rollator,Rollator walker with seat,4 wheels rollator,Rollator china,Rollator walker folding
Foshan Oscar Medical Instrument CO.,LTD , https://www.fsoscarmed.com